Introduction
Metformin is a widely prescribed medication for individuals with type 2 diabetes, and for good reason. It has been shown to effectively control blood sugar levels, reduce the risk of diabetes-related complications, and even promote weight loss in some cases. However, like any medication, metformin comes with potential side effects, one of which is the development of low blood sugar levels, also known as hypoglycemia.
Hypoglycemia can be a serious condition if left untreated, as the brain and other vital organs rely on a steady supply of glucose for proper functioning. Understanding the relationship between metformin and hypoglycemia is crucial for diabetic patients to ensure their safety and well-being while managing their condition effectively.
Understanding Hypoglycemia
Hypoglycemia occurs when the glucose (sugar) level in the blood drops below the normal range, typically defined as less than 70 mg/dL (3.9 mmol/L). This condition can manifest with a range of symptoms, including shakiness, dizziness, sweating, confusion, anxiety, headaches, and, in severe cases, seizures or loss of consciousness.
The symptoms of hypoglycemia can vary from person to person, and some individuals may not experience any noticeable signs until their blood sugar levels become dangerously low. Diabetic patients need to be aware of their unique hypoglycemia symptoms and recognize them early to take appropriate action.
Metformin and Hypoglycemia Risk
Mechanism of Action
Metformin is an oral medication in the biguanide class. It works by decreasing the amount of glucose produced by the liver (a process known as gluconeogenesis) and increasing the sensitivity of the body’s cells to insulin, allowing them to utilize glucose more effectively.
While metformin does not directly lower blood sugar levels, its mechanism of action can indirectly decrease blood glucose concentrations, especially when combined with other factors such as dietary changes, physical activity, or other diabetes medications.
Risk Factors
It’s important to note that the risk of hypoglycemia with metformin alone is relatively low, especially in individuals with type 2 diabetes. However, certain factors can increase the likelihood of experiencing low blood sugar levels:
- Combination with other diabetes medications: Taking metformin with insulin or other medications that increase insulin levels or enhance insulin sensitivity (such as sulfonylureas or meglitinides) can heighten the risk of hypoglycemia.
- Skipping meals or prolonged fasting: Metformin reduces the amount of glucose the liver produces. If you skip meals or go for extended periods without eating, your blood sugar levels may drop too low.
- Alcohol consumption: Consuming alcohol while taking metformin can increase the risk of hypoglycemia, as alcohol can interfere with the body’s ability to regulate blood sugar levels.
- Strenuous physical activity: Engaging in intense or prolonged physical activity without adjusting your medication or diet can lead to a drop in blood sugar levels.
- Impaired kidney or liver function: Metformin is primarily eliminated through the kidneys, and individuals with impaired kidney or liver function may have reduced clearance of the drug, increasing the risk of hypoglycemia.
It is essential to discuss these risk factors with your healthcare provider and take appropriate precautions to minimize the chances of experiencing hypoglycemia while taking metformin.
Managing Hypoglycemia with Metformin
Prevention
Preventing hypoglycemia is the best approach to managing this potential side effect of metformin. Here are some strategies to consider:
- Follow a balanced diet: Maintain a consistent eating schedule and avoid skipping meals. Consult a registered dietitian or nutritionist to develop a meal plan that suits your needs and helps regulate your blood sugar levels.
- Exercise regularly: Regular physical activity can improve insulin sensitivity and help control blood sugar levels. However, monitoring your blood glucose levels before, during, and after exercise is essential to adjust your medication or food intake accordingly.
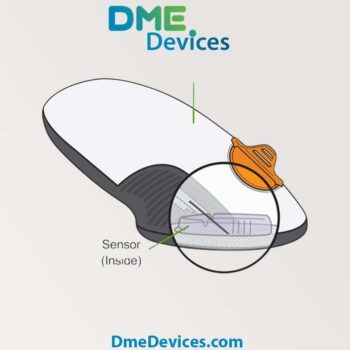
- Monitor blood sugar levels: Regularly checking your blood sugar levels using a glucometer can help you identify potential hypoglycemic episodes early and take corrective action.
- Adjust medication dosages: If you experience frequent hypoglycemia, your healthcare provider may recommend adjusting your metformin dosage or the timing of your medication to accommodate your lifestyle and dietary habits better.
- Wear medical identification: Consider wearing a medical alert bracelet or carrying some form of identification that indicates you have diabetes and are taking metformin in case you experience a severe hypoglycemic event and require medical assistance.
Treatment
If you experience symptoms of hypoglycemia while taking metformin, it’s crucial to act promptly to raise your blood sugar levels. Here are some steps to follow:
- Consume a fast-acting carbohydrate source: Glucose tablets, fruit juice, hard candies, or sugary drinks can provide a quick boost in blood sugar levels. The recommended dose is 15-20 grams of carbohydrates.
- Recheck your blood sugar levels: After 15-20 minutes, recheck your blood sugar levels either with blood glucose monitor or continuous glucose monitoring system such as CGM. If they remain low, consume another 15 grams of carbohydrates.
- Eat a balanced snack or meal: Once your blood sugar levels have stabilized, consume a balanced snack or meal containing carbohydrates, proteins, and healthy fats to help maintain stable blood sugar levels.
- Seek medical attention: In severe cases of hypoglycemia, where the individual is unable to consume food or drink or has lost consciousness, immediate medical attention may be required. Emergency treatments may be necessary, such as administering glucagon or intravenous glucose.
It’s essential to discuss any episodes of hypoglycemia with your healthcare provider, as they may need to adjust your metformin dosage or consider alternative treatment options to manage your diabetes better while minimizing the risk of low blood sugar levels.
Numerical Facts and Figures
To better understand the impact of hypoglycemia and the importance of managing it effectively, consider the following numerical facts and figures:
- According to the American Diabetes Association, hypoglycemia is a blood glucose level below 70 mg/dL (3.9 mmol/L).
- Severe hypoglycemia (blood glucose levels below 54 mg/dL or 3.0 mmol/L) can lead to seizures, coma, or even death if left untreated.
- A study published in the journal Diabetes Care found that individuals with type 2 diabetes taking metformin alone had a relatively low risk of hypoglycemia, with an incidence rate of 0.6 events per 100 person.
- However, the risk of hypoglycemia increased significantly when metformin was combined with other diabetes medications, such as sulfonylureas (incidence rate of 7.3 events per 100 person) or insulin (incidence rate of 19.9 events per 100 person).
- According to the Centers for Disease Control and Prevention (CDC), approximately 282,000 emergency room visits and 180,000 hospitalizations occur annually in the United States due to hypoglycemia among individuals with diabetes.
These statistics highlight the importance of being aware of the potential risk of hypoglycemia and taking appropriate measures to prevent and manage it effectively, especially when taking metformin in combination with other diabetes medications.
Conclusion
Metformin is a widely used and effective medication for managing type 2 diabetes, but patients must be aware of the potential risk of hypoglycemia, or low blood sugar levels, especially when combined with other risk factors or medications. By understanding the mechanisms behind this potential side effect, recognizing the signs and symptoms of hypoglycemia, and implementing preventive strategies, diabetic patients can safely and effectively manage their condition while minimizing the risk of complications.
It’s crucial to work closely with your healthcare provider, follow a balanced diet, exercise regularly, and monitor your blood sugar levels consistently. By taking a proactive approach and being vigilant, you can enjoy the benefits of metformin while minimizing the risk of experiencing hypoglycemia and maintaining optimal health and well-being.
Remember, managing diabetes is a journey, and with the proper knowledge, support, and mindset, you can navigate it successfully and live a fulfilling life.













Write a comment
Your email address will not be published. All fields are required