Does the Apple Watch Series 7 Monitor Glucose Levels for Diabetes Management?
Introduction
Diabetes is a chronic condition that affects millions of people worldwide, and proper management is crucial for maintaining overall health and preventing complications. In recent years, wearable technology has emerged as a valuable tool for individuals with diabetes, offering convenient monitoring and tracking capabilities. The Apple Watch, in particular, has garnered attention for its potential in diabetes management. With the release of the Apple Watch Series 7, many users are wondering if this latest iteration can monitor glucose levels, a critical aspect of diabetes care.
Apple Watch and Glucose Monitoring
Current Limitations
As of now, the Apple Watch Series 7 does not have a built-in feature that directly measures or monitors blood glucose levels. The watch relies on external devices, such as continuous glucose monitors (CGMs) or blood glucose meters, to obtain glucose data. While this may seem like a limitation, it is important to understand the challenges associated with non-invasive glucose monitoring.
Traditionally, glucose monitoring has required drawing a small amount of blood through finger pricks or implanted sensors. This invasive approach has been the most accurate and reliable method for measuring glucose levels. However, researchers have been exploring non-invasive techniques, such as using light or electrical signals to measure glucose levels through the skin. While promising, these technologies are still in their infancy and face several challenges, including accuracy, calibration, and interference from various factors like skin composition and hydration levels.
Third-Party App Integration
While the Apple Watch itself cannot measure glucose levels, it can integrate with third-party apps that connect to compatible CGMs or glucose meters. These apps can display real-time glucose readings, trends, and alerts on the watch face, allowing users to monitor their glucose levels conveniently from their wrists.
One popular app for diabetes management on the Apple Watch is Dexcom's G6 CGM app. This app connects to the Dexcom G6 CGM system, which consists of a small sensor worn on the body that continuously measures glucose levels in the interstitial fluid (the fluid between cells). The app displays glucose readings, trends, and alerts on the Apple Watch, enabling users to quickly glance at their levels and take appropriate actions, such as administering insulin or consuming carbohydrates.
Future Developments
Apple has been actively exploring ways to incorporate non-invasive glucose monitoring technology into its devices. Rumors and reports suggest that the company is working on developing a sensor that could potentially measure glucose levels through the skin, without the need for finger pricks or implanted devices. This technology, if successfully developed, could revolutionize diabetes management by providing a seamless and convenient way to monitor glucose levels.
However, it's important to note that non-invasive glucose monitoring is a complex challenge, and it's uncertain when or if Apple will be able to overcome the technical hurdles and successfully integrate this technology into future Apple Watch models. Factors such as accuracy, reliability, and regulatory approvals need to be addressed before such a feature can be widely adopted for diabetes management.
Diabetes Management with the Apple Watch
Activity and Exercise Tracking
While the Apple Watch Series 7 may not directly monitor glucose levels, it offers valuable features for diabetes management. The watch's activity tracking capabilities can help individuals with diabetes stay active and monitor their exercise routines, which are essential for maintaining healthy blood sugar levels and overall well-being.
Regular physical activity has been shown to improve insulin sensitivity, which can help regulate blood sugar levels and reduce the risk of complications associated with diabetes. The Apple Watch Series 7 can track various activities, such as walking, running, cycling, and swimming, providing valuable data on calories burned, distance covered, and heart rate. This information can be used to adjust insulin doses, plan meals, and optimize exercise routines for better blood sugar control.
Nutrition and Calorie Tracking
The Apple Watch also integrates with various apps that allow users to track their food intake, calorie consumption, and nutrition information. This can be particularly useful for individuals with diabetes, as monitoring carbohydrate intake is crucial for managing blood sugar levels.
Apps like MyFitnessPal and Lose It! can be synced with the Apple Watch, enabling users to log their meals and snacks directly from their wrists. These apps provide detailed nutritional information, including carbohydrate counts, which can help individuals with diabetes make informed decisions about their food choices and insulin dosages.
Reminders and Alerts
The Apple Watch can be set up to provide reminders and alerts for various health-related tasks, such as taking medication, checking glucose levels, or engaging in physical activity. These reminders can be invaluable for individuals with diabetes, helping them stay on top of their daily routines and maintain better control over their condition.
For example, users can set medication reminders on the Apple Watch to ensure they take their insulin or other diabetes medications at the appropriate times. They can also set alerts to check their glucose levels at regular intervals or before engaging in physical activity. Additionally, the watch can provide reminders for scheduling doctor appointments or refilling prescriptions, ensuring that individuals with diabetes stay proactive in managing their condition.
Mindfulness and Stress Management
The Impact of Stress on Diabetes
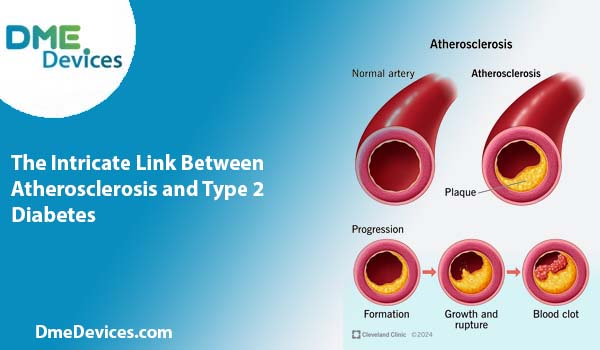
Stress can have a significant impact on individuals with diabetes, as it can affect blood sugar levels and potentially contribute to complications. When under stress, the body releases hormones like cortisol and adrenaline, which can cause an increase in blood sugar levels. Additionally, stress can lead to unhealthy coping mechanisms, such as overeating or neglecting self-care routines, further exacerbating the challenges of diabetes management.
Mindfulness Features on the Apple Watch
The Apple Watch Series 7 offers several mindfulness features that can help individuals with diabetes manage stress and promote overall well-being. The Breathe app, for instance, guides users through simple breathing exercises designed to reduce stress and promote relaxation. This can be particularly beneficial for individuals with diabetes, as stress management is an integral part of maintaining healthy blood sugar levels.
Additionally, the Apple Watch integrates with various third-party mindfulness apps, such as Calm and Headspace, which provide guided meditations, sleep stories, and other resources to cultivate mindfulness and reduce stress. Incorporating these practices into daily routines can help individuals with diabetes better cope with the challenges and emotional aspects of managing their condition.
Connectivity and Telehealth
Remote Monitoring and Telemedicine
The Apple Watch's connectivity features can also be leveraged for remote monitoring and telemedicine in diabetes care. With the rise of telehealth services, individuals with diabetes can potentially share their glucose data, activity levels, and other health metrics with their healthcare providers remotely.
This can enable healthcare professionals to monitor their patients' progress, identify potential issues, and provide timely interventions or adjustments to treatment plans without the need for in-person visits. Additionally, telehealth consultations can be conducted through video calls or messaging applications, allowing individuals with diabetes to receive personalized guidance and support from the comfort of their own homes.
Integration with Electronic Health Records
As technology continues to advance, there is potential for the Apple Watch to integrate with electronic health records (EHRs) and other healthcare systems. This integration could enable seamless sharing of glucose data, activity levels, and other relevant health information between individuals with diabetes and their healthcare providers.
By consolidating data from various sources, including wearable devices like the Apple Watch, healthcare professionals can gain a more comprehensive understanding of their patients' conditions and make more informed decisions about treatment plans and lifestyle recommendations.
Conclusion
While the Apple Watch Series 7 does not have a built-in feature for directly monitoring glucose levels, it can still be a valuable tool for individuals with diabetes. By integrating with third-party apps and leveraging its activity and nutrition tracking capabilities, the Apple Watch can assist in managing various aspects of diabetes care.
As technology continues to evolve, it is possible that future Apple Watch models may incorporate non-invasive glucose monitoring capabilities, further enhancing their usefulness for individuals with diabetes. However, even without this specific feature, the Apple Watch Series 7 offers a range of functionalities that can contribute to better diabetes management, including mindfulness practices, reminders, and connectivity with healthcare providers.
Ultimately, the key to successful diabetes management lies in a comprehensive approach that combines various tools and strategies, such as monitoring glucose levels, maintaining a healthy diet and exercise routine, managing stress, and staying connected with healthcare professionals. The Apple Watch Series 7, when utilized in conjunction with other diabetes management tools and guidance from healthcare providers, can be a valuable addition to an individual's diabetes care toolkit.