Showering with the FreeStyle Libre 3 Continuous Glucose Monitoring System
Table of Content:
- Introduction
- Water Resistance and Durability
- Benefits of Continuous Glucose Monitoring During Water Activities
- Importance of Continuous Glucose Monitoring for Diabetes Management
- Conclusion
Introduction
Diabetes management is a constant process that requires diligent monitoring and adjustment of various factors, including glucose levels, insulin dosages, and lifestyle choices. The FreeStyle Libre 3 continuous glucose monitoring (CGM) system has revolutionized the way individuals with diabetes can track their glucose levels, providing real-time data and insights that enable better management of this chronic condition. One of the most frequently asked questions about this device is whether it is safe to shower or bathe while wearing it. As a professional diabetes expert, I can assure you that the FreeStyle Libre 3 is indeed water-resistant and can be worn while showering or participating in other water-related activities.
Water Resistance and Durability
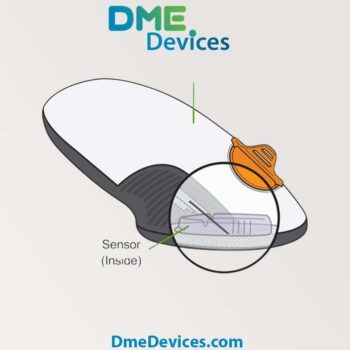
The FreeStyle Libre 3 sensor is designed to withstand exposure to water, making it suitable for everyday activities, including showering, bathing, and swimming. The sensor is water-resistant up to a depth of 1 meter (3 feet) for up to 30 minutes. This means that you can safely wear the sensor while taking a shower, enjoying a relaxing bath, or even engaging in recreational water activities like swimming without the need to remove or replace it.
The water-resistance of the FreeStyle Libre 3 is achieved through a combination of advanced engineering and meticulous design. The sensor is encased in a durable, water-resistant housing that protects the internal components from moisture and water exposure. Additionally, the adhesive used to secure the sensor to the skin is specially formulated to maintain its adhesive properties even when exposed to water.
Precautions and Best Practices
While the FreeStyle Libre 3 is water-resistant, it is important to follow some best practices to ensure its longevity and optimal performance:
- Avoid prolonged submersion: Although the sensor can withstand water exposure for up to 30 minutes, it is recommended to avoid submerging it for extended periods beyond the recommended time frame. Prolonged submersion may increase the risk of water seeping into the device and potentially compromising its functionality.
- Avoid extreme temperatures and humidity: Avoid exposing the sensor to hot tubs, saunas, or steam rooms, as the high temperatures and humidity levels may damage the device or cause discomfort during wear.
- Gentle drying: After exposure to water, gently pat the sensor dry with a clean towel. Avoid rubbing or scrubbing the sensor, as this may compromise the adhesive and lead to premature detachment.
- Do not remove when wet: It is recommended not to attempt to remove the sensor while it is wet, as this may cause discomfort or damage the adhesive. Allow the sensor to dry completely before considering removal.
Benefits of Continuous Glucose Monitoring During Water Activities
The ability to wear the FreeStyle Libre 3 while showering or participating in water-based activities offers several benefits for individuals with diabetes:
- Uninterrupted glucose monitoring: By keeping the sensor on during showering or swimming, you can continue to monitor your glucose levels without interruption, ensuring better management of your diabetes. This is particularly important for individuals with type 1 diabetes or those prone to rapid fluctuations in blood sugar levels, as even a short period without monitoring can lead to potentially dangerous situations.
- Convenience and ease of use: The water-resistant feature eliminates the need to remove and reapply the sensor constantly, providing a seamless and convenient experience. This can be especially beneficial for individuals with mobility challenges or those who find frequent sensor replacements challenging.
- Improved hygiene: Wearing the sensor during showering or bathing allows for better personal hygiene without compromising your glucose monitoring. Maintaining good hygiene is crucial for individuals with diabetes, as they may be more susceptible to infections and skin-related complications.
- Peace of mind: Knowing that you can continue to monitor your glucose levels during water activities can provide a sense of security and peace of mind, allowing you to enjoy these activities without worrying about potential complications or disruptions in your diabetes management routine.
Importance of Continuous Glucose Monitoring for Diabetes Management
Continuous glucose monitoring (CGM) has become an indispensable tool in the management of diabetes, offering numerous benefits that traditional fingerstick glucose monitoring cannot provide. By providing real-time glucose data and trends, CGM systems like the FreeStyle Libre 3 allow individuals with diabetes to make more informed decisions about their treatment and lifestyle choices.
One of the key advantages of CGM is the ability to detect and respond to potential hypoglycemic (low blood sugar) or hyperglycemic (high blood sugar) events before they become severe. These conditions can be life-threatening if left untreated, and early intervention can prevent serious complications. CGM systems can alert users when their glucose levels are approaching dangerous levels, allowing them to take corrective actions promptly.
CGM data also provides valuable insights into how various factors, such as food, exercise, and medication, affect an individual's glucose levels. By analyzing these trends, individuals with diabetes and their healthcare providers can make more informed decisions about adjusting insulin dosages, dietary choices, or exercise regimens to better manage their condition.
Facts and Figures
The importance of effective diabetes management cannot be overstated, as the consequences of uncontrolled blood sugar levels can be severe. According to the International Diabetes Federation (IDF), in 2021, approximately 537 million adults (20-79 years) were living with diabetes worldwide, and this number is projected to rise to 783 million by 2045. Diabetes is a leading cause of various complications, including cardiovascular disease, kidney disease, blindness, and lower limb amputations.
Numerous studies have demonstrated the effectiveness of continuous glucose monitoring in improving glycemic control and reducing the risk of complications associated with diabetes. A systematic review and meta-analysis published in the Journal of the American Medical Association (JAMA) in 2022 found that the use of CGM systems was associated with a significant reduction in HbA1c levels (a measure of long-term blood sugar control) compared to traditional self-monitoring of blood glucose.
Furthermore, research has shown that CGM can improve quality of life and reduce the burden of diabetes management. A study published in Diabetes Technology & Therapeutics in 2020 reported that individuals using CGM systems experienced improved treatment satisfaction, reduced diabetes-related distress, and better overall well-being compared to those using traditional glucose monitoring methods.
Conclusion
The FreeStyle Libre 3 continuous glucose monitoring system is a game-changer for individuals with diabetes, offering water-resistant capabilities that allow for uninterrupted glucose monitoring during showering and other water-based activities. By following the recommended precautions and best practices, you can enjoy the benefits of this innovative technology while maintaining optimal sensor performance and personal hygiene.
Continuous glucose monitoring has become an essential tool in the management of diabetes, providing real-time data, trend analysis, and early warning systems for potential complications. The ability to wear the FreeStyle Libre 3 during water activities not only enhances convenience and hygiene but also contributes to better overall diabetes management and improved quality of life.
As a professional diabetes expert, I strongly encourage individuals with diabetes to explore the potential benefits of continuous glucose monitoring systems like the FreeStyle Libre 3. By embracing these advanced technologies and maintaining a proactive approach to diabetes management, individuals can take control of their condition and live healthier, more fulfilling lives.